What is CBT for Eating Disorders?
How does CBT work for eating disorders?
What is CBT and why is it so effective for eating disorder treatment? By the end of this article you’ll understand what CBT is, how it works for my own real-life clients with eating disorders, and what you can expect if you’re heading into CBT-focused therapy.
CBT stands for cognitive-behavioral therapy, and by many eating disorder professionals is considered the gold standard treatment for anorexia, bulimia, and binge eating disorder.
Why? Because it works, and usually, it works fast!
Though not all treatments are effective for all clients, CBT is an evidenced based practice. In other words, CBT is backed by an abundance of clinical research pointing to the conclusion that it is helpful and reliable for many.
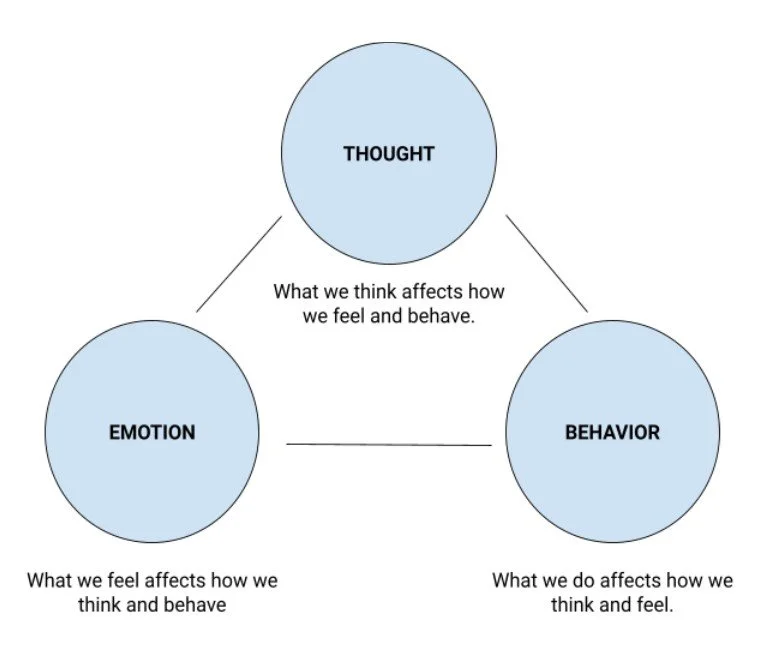
Let me break it down a bit. Cognitive behavioral therapy operates from the perspective that changing your thoughts can have a powerful impact on changing your emotional state, as well as your behaviors that might be harmful. Essentially, to change your eating disorder behaviors we need to change the thoughts that lead to them!
To give you a better picture of what that means in action, I’d like to tell you a story:
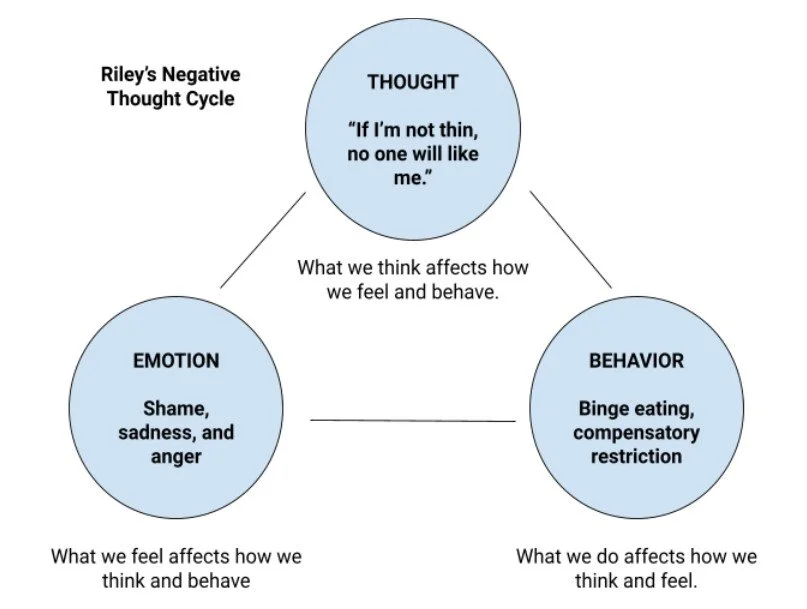
Riley has been dealing with eating problems for the past two years, and has been working with a therapist who specializes in eating disorders and CBT. A key focus of her therapy sessions has been talking about the thoughts she has about food and her body. They also talk about what triggers these thoughts, how they make her feel, and which disordered food behaviors they lead to.
One common thought Riley has is, “If I’m not thin, no one will ever love me.” Pretty intense, right! But super common for those of us with disordered eating. With her therapist, Riley notes that this thought often brings up feelings of shame, sadness, and anger. When Riley feels overwhelmed by shame and other emotions, she tends to reach out for food to provide her comfort, and this can very often lead to a binge episode. Subsequently, Riley becomes even more ashamed that she binged, and heavily restricts her food the next day to compensate – reinforcing the thought “If I’m not thin, no one will like me.”
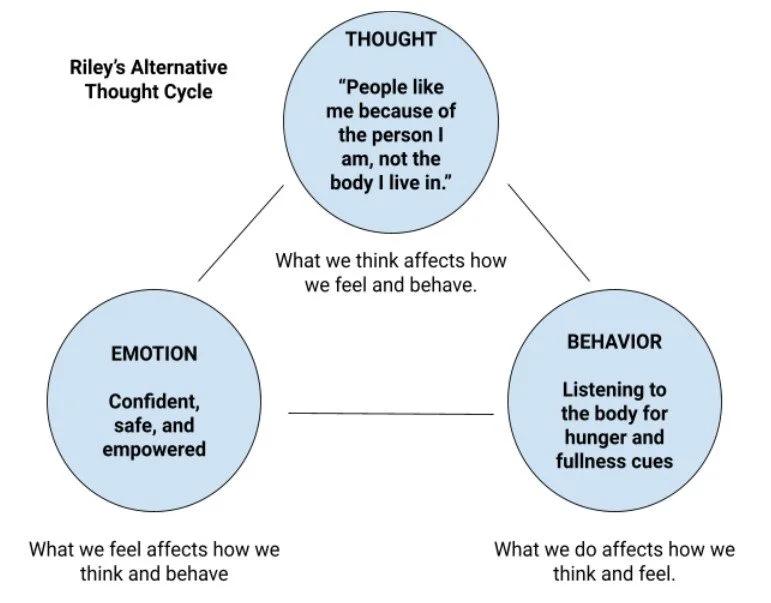
I wonder what might happen if Riley’s unhelpful thought was different. If Riley was able to change her belief from “If I’m not thin, no one will like me,” to “People like me because of the person I am, not the body I live in,” her life experience could dramatically change. Instead of feelings of shame, Riley might feel confident, safe, even empowered. Instead of binging and restricting, Riley might give herself permission to listen to body when it comes to food. At the beginning of therapy, this kind of change likely felt impossible, but with the roadmap that CBT provides, she is getting closer and closer to finding new thoughts and beliefs that support her recovery.
Riley’s story illustrates a very common thought cycle that I encounter with my eating disorder clients. I hope from her example you can begin to understand how disordered eating is a vicious and self-perpetuating cycle – very often fueled by unhelpful, irrational, and untrue thoughts.
Working with a CBT therapist who also specializes in eating disorders you can begin to identify how these thoughts impact you uniquely. In my CBT work, I aim to guide client’s to a place of self-awareness and insight about their own cycle of thoughts, emotions, and behaviors. CBT helps to create your very own therapy toolkit, providing templates, models, and structured practices to take with you outside of session to facilitate the process of rewiring your thought patterns. CBT is more than just talk therapy – it is action and education oriented (i.e. you’ll learn a lot about your brain, you’ll be given the tools to change what isn’t working for you!).
Cognitive behavioral therapy is a “transdiagnostic” approach; this just means it works for all sorts of mental health diagnoses, not just eating disorders. This can be super helpful if you’re struggling with depression, and/or anxiety along with disordered eating. However, there is a version of CBT that was developed specifically for eating disorders. It is called Cognitive Behavioral Therapy Enhanced or CBT-E; and this is what I use most in my practice!
CBT-E is a modified version of traditional CBT, developed with the unique issues presented by eating disorders in mind. It is a highly structured model that provides evidenced based skills and practices to recover from disordered eating. Allow me to explain how this works in my own therapy practices through exploring the first three stages of CBT-E.
Stage 1: Starting Well
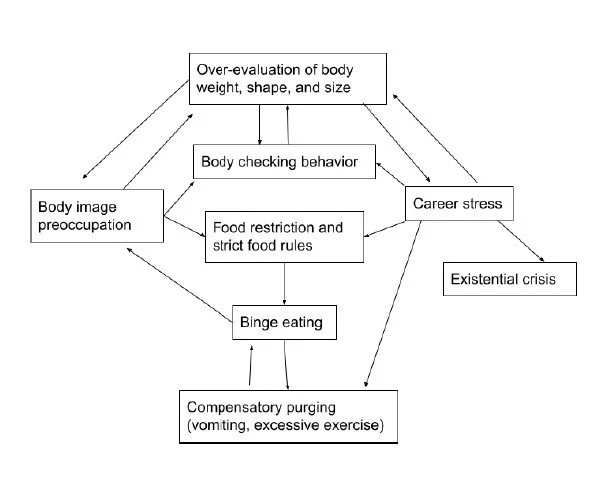
This is our “getting to know you” phase. We’ll spend our first session talking about your background – including gathering information about your eating disorder, how and when it developed, other mental health struggles you might be experiencing, and your personal/family history. We’ll also collaborate to create your personal “formulation” – this is a diagram of the processes (behaviors, thoughts, emotions, places, people, etc!) that appear to be keeping your eating disorder around. You can take a look at an example below:
Example formulation representing a client with bulimia
Other aspects of stage one include learning the facts about eating disorders, learning to self-monitor your food behaviors, and begin implementing small changes to the way you’re eating and engaging with your body.
Stage 2: Taking Stock and Designing the Rest of Treatment
In this stage, we pause to evaluate early progress and changes made in stage one. This gives us information on how to move forward and personalize your treatment according to your needs. We’ll discuss what is working, what barriers are coming up, and we’ll review our formulation to make changes if necessary.
Stage 3: Body Concern, Body Checking, and Disordered Mindsets
Here, we start to address each process identified in your formulation. For most eating disorders, at the heart of the problem is the “over-evaluation” of shape, weight, and control. Essentially, this is the idea that your value is attached to your body shape and weight, and the distorted belief that you should have control over your body shape and weight. Debunking and rewiring these beliefs and mindsets is the linchpin of CBT! If we can change the way we think about body shape, weight, and control, behavioral and emotional change is sure to follow.
Stages 1-3 tend to be standard for most of my eating disorder clients. The following stages are tailored specifically to an individual’s need. For example, some clients find that emotional states or situations trigger eating disorder behaviors. Others find that beliefs seemingly unrelated to their eating disorder are pivotal in their recovery journey. We’ll work together to discover what needs to be addressed.
So, now what?
If you’re reading this, it is probably your sign that eating disorder therapy may be the right move for you. I hope this article demystified what it would be like to begin eating disorder treatment from a cognitive behavioral therapy perspective. It can be so intimidating when you finally decide to confront your eating disorder and if you’re feeling overwhelmed, I understand.
In looking for a therapist you want to make sure they're the right fit, both personally and professionally! That’s exactly why I offer a free 15 minute consultation call before you book an appointment with me. I am happy to answer any questions you might have about therapy with me, other types of therapy I offer, and my own eating disorder recovery journey.
There is a way out of disordered eating, and cognitive behavioral therapy might be your way! Let’s connect and find your path to recovery.
Citation
Fairburn, C. G. (2008). Cognitive Behavior Therapy and Eating Disorders. The Guilford Press.